What is Achilles Tendonitis?
The achilles tendon is one of the most important tendons in our bodies, yet it is one that can be suseptible to injury. Today, we’re going to discuss the achilles tendon, the most common issues that can affect it and how these are treated.
What and where is the achilles tendon?
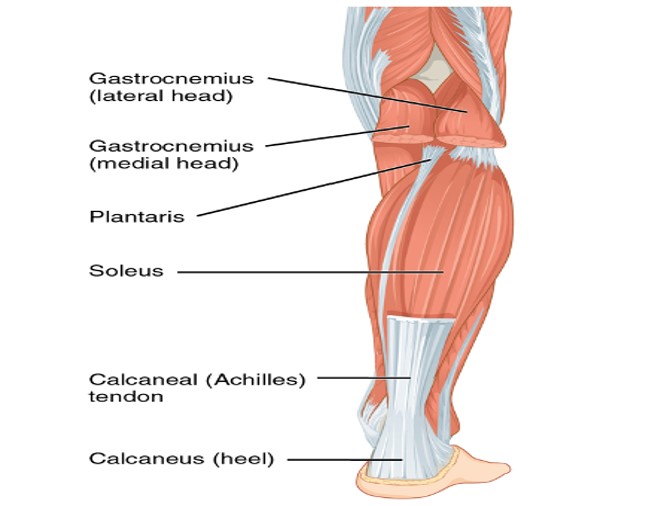
Tendons are fibrous connective tissue that attach muscles to bones, and when contracted enable the movement of the bones it attaches to.
The achilles tendon is the tendon that attaches the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus).
The achilles tendon is the simultaneously the biggest and strongest tendon in the body, this is primarily due to the workload the tendon is placed under.
This incredible tendon is responsible for producing movements that enable you to walk, run and jump.
Despite the remarkable resilience of our achilles, often times the demand we place the tendon under can be too much, inevitably resulting in injury.
What is achilles tendinopathy?
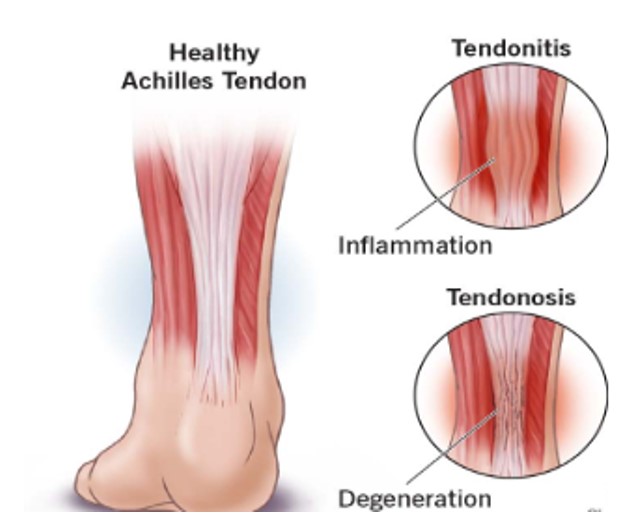
Achilles tendinopathy is an umbrella term for conditions affecting the achilles including tendinitis or tendinosis.
Tendinitis refers to the inflammation of the tendon; this can be present without any damage having occurred to the tendon fibers. In such circumstances the tendon may become swollen, warm and red. Conversely, tendinosis refers to the damage and disorganization of the tendon fibers, in such instances the tendon may feel stiff and rubbery. An achilles may be concurrently affected by both tendinitis and tendinosis.
How do I know if I have achilles tendinopathy?
Common symptoms that are associated with achilles tendinopathy include: pain, inflammation, swelling, tenderness to touch, stiffness and tendon thickening.
One or more of these symptoms being present may indicate a tendinopathy. These symptoms will often lead to difficulty walking for extended periods of time, as well as trouble walking up hills and/or stairs, running and jumping.
Nevertheless, these symptoms may also be associated with other pathologies that affect the achilles such as a tear or rupture, retrocalcaneal bursitis, paratendinitis, calcaneal stress fracture, Haglund deformity and Sever’s disease.
Treatments for these pathologies differ from that of tendinopathy, therefore it is important to see a podiatrist to have a definitive diagnosis.
How is achilles tendinopathy diagnosed?
Achilles tendinopathy can be diagnosed by a proper medical history evaluation, patient symptom evaluation, clinical exams which include palpation, range of motion tests, and muscle strength and flexibility tests.
This will be coupled with radiographic and ultrasound imaging to confirm the findings gathered during the consultation.
Once a definitive diagnosis is made, it is important to have the reason for the injury investigated to prevent reinjury.
What causes achilles tendinopathy?
There are three predominant causes of achilles tendinopathy these consist of:
1. Abrupt increased tendon loading
Tendons are generally able to withstand the day-to-day workload we put them under, however when engaging in activities our tendons have not been conditioned to perform, this can often result in tendinopathy.
Examples of this may include, sudden increases in running or jumping or working in an environment where you’re expected to walk uphill for extended periods.
2. Tightness in the calf muscles
Tightness in the calf muscles can lead to tension being placed on the achilles. This tension can result in a pull at the insertion point of the achilles on the heel bone, resulting in inflammation and pain.
3. Biomechanical and structural causes
Sometimes the structure of our feet may lead to increased tension being place on the achilles. The achilles can be continually strained due to way we walk, this can be a result of a restriction in the ankle, knee or hip.
4. Other risk factors include:
Steroid use, unsupportive footwear, high blood pressure, obesity and certain antibiotic use.
What treatments are available at Hurst Podiatry to treat achilles tendinopathy?
1. Relative Rest/Moon boot – Resting will always be advised when recovering from any tendinopathy. This can be enhanced if needed by the use of a moon boot. This may not be practically possible due to the type of work you do but reducing the overall load on the tendon throughout the day will aid in recovery.
2. Anti-inflammatory medication – These medications can temporarily reduce the pain and discomfort experienced. Medications such as Nurofen, Voltaren tablets and topical gels, Advil and Fisiocrem topical rub. It is worth noting use of some anti inflammatory medications can slow down Achilles’ tendon healing.
3. Stretches and eccentric exercises – Calf and hamstring stretches can help ensure the tendon remains loose and mobile. This can be particularly helpful at the start of the day when the tendon is feeling tight and at the end. Eccentric exercises have been proven to be effective strengthening exercises when rehabilitating the achilles from tendinopathy and a range of other tendon problems.
4. Heel lifts – Heel lifts can help decrease the load on the tendon when walking, this can aid reduce pain and discomfort during the initial stages of recovery.
5. Orthotics – Orthotics are effective devices to treat achilles tendinopathy when the achilles is placed under tension as result of the foots structure and alignment.
6. Shockwave therapy – Shockwave therapy is an effective tool to stimulate healing. The shockwave device works by increasing blood flow, muscle repair, muscle regeneration and bone repair.
7. K-laser therapy – low level laser therapy has proven to be effective for many conditions affecting muscles, tendons and ligaments. Laser therapy works by increasing blood flow, increasing oxygen and speeding up the rate at which the cells recover. Here at Hurst Podiatry, we have the latest model of the K-laser Cube Plus 30 which has been providing fast and effective results after just the first treatment.
8. Prolotherapy – Prolotherapy is an injection therapy, whereby an irritant is injected around the tendon and the ligament attachments which stimulates tendon healing and strengthen the ligaments attached.
Are you experiencing pain in your achilles?
If any of what we’ve talked about today sounds familiar to you and you’re in Melbourne’s Eastern area, book in to see us at our podiatry clinic. We have 3 locations in Victoria – in Healesville and Kilsyth – and a team of highly experienced podiatrists who are here to help you take care of your feet.
Call 03 5901 2216 or book online here.