What is Tarsal Tunnel Syndrome?
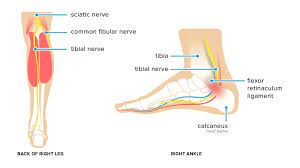
Tarsal tunnel syndrome, a lesser-known but potentially debilitating condition, affects the foot by compressing the tibial nerve in the ankle, resulting in pain and numbness. This condition leads to symptoms that are very similar to carpal tunnel syndrome.
In this guide, we will discuss the key aspects of tarsal tunnel syndrome, from symptoms to treatment options. We aim to provide a deeper understanding of tarsal tunnel syndrome, aiding those who may be affected or at risk and seeking guidance for managing this challenging foot ailment.
What is tarsal tunnel syndrome and how does it affect the foot?
Tarsal tunnel syndrome is a condition that affects the foot, and it arises from the compression or irritation of the tibial nerve as it passes through a narrow space known as the tarsal tunnel, which is situated along the inner side of the ankle. This condition can cause discomfort in the foot, manifesting as pain, tingling, and numbness, which are sensations akin to those experienced in carpal tunnel syndrome, but localized in the foot.
The areas of the foot most commonly impacted include the heel, arch, and sole. These symptoms tend to worsen during extended periods of standing or walking, making it important to understand the condition and its underlying causes.
What are the signs and symptoms of tarsal tunnel syndrome?
Tarsal tunnel syndrome is characterized by a range of signs and symptoms that can impact the foot and ankle. These include:
- Foot Pain: Individuals with tarsal tunnel syndrome often experience pain in the affected foot. This pain can vary in intensity, ranging from mild discomfort to severe and debilitating pain.
- Tingling Sensations: Many people with this condition report sensations of tingling or pins and needles in the foot and ankle. These sensations can be sporadic or persistent.
- Numbness: Numbness in the foot, particularly in the sole and toes, is a common symptom. It can affect mobility and sensation in the foot.
- Burning Sensation: Some individuals describe a burning sensation in the affected area, which can be quite uncomfortable.
- Electric Shock-like Sensations: In some cases, people may feel as if they are experiencing electric shock-like sensations in the foot and ankle.
- Worsening with Activity: Symptoms often worsen with activities that involve prolonged standing, walking, or running. This can make it challenging to engage in these activities comfortably.
- Weakness: Tarsal tunnel syndrome can lead to weakness in the foot and ankle. This weakness may make it difficult to flex or move the toes.
It’s important to note that the severity and combination of these symptoms can vary from person to person. If you or someone you know is experiencing these symptoms, it’s essential to seek professional medical evaluation and diagnosis by a podiatrist to determine the best course of treatment.
What are the causes and risk factors associated with tarsal tunnel syndrome?
Tarsal tunnel syndrome can have various causes and risk factors that contribute to its development. Understanding these factors is crucial for both prevention and effective management. The primary causes and risk factors include:
- Nerve Compression: The most common cause of tarsal tunnel syndrome is the compression of the tibial nerve within the tarsal tunnel. This compression can be due to a variety of factors.
- Flat Feet (Pes Planus): Flat feet, where the arch of the foot is reduced or absent, can increase pressure on the tibial nerve as it passes through the tarsal tunnel. This pressure can lead to compression and the onset of symptoms.
- Ankle Injuries: Ankle sprains or fractures that result in swelling and inflammation in the tarsal tunnel can contribute to tarsal tunnel syndrome.
- Overpronation: Overpronation, which is the excessive inward rolling of the foot during walking, can lead to increased strain on the tibial nerve.
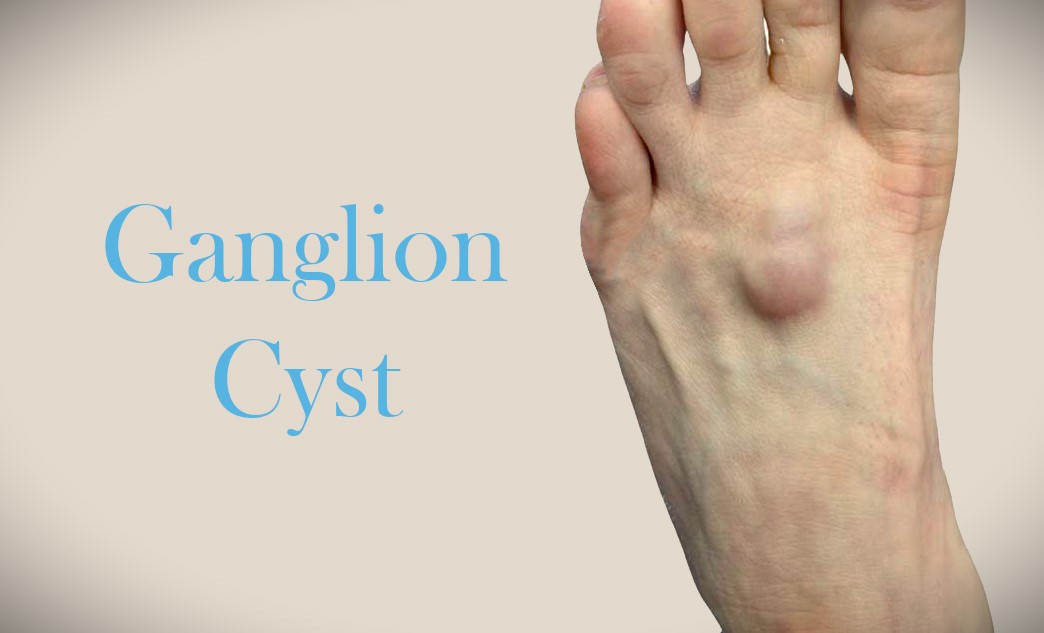
- Cysts and Masses: The presence of cysts or masses within the tarsal tunnel can directly impinge on the tibial nerve, causing compression and symptoms of the syndrome.
- Systemic Conditions: Certain systemic conditions such as diabetes and arthritis can increase the risk of nerve compression in the tarsal tunnel.
- Prior Injuries: Previous injuries to the ankle, particularly those resulting in scar tissue formation, can create pressure on the tibial nerve and contribute to tarsal tunnel syndrome.
- Foot Deformities: Specific foot deformities, including those that affect the structure or alignment of the foot, can increase the risk of nerve compression.
How is tarsal tunnel syndrome diagnosed?
The diagnosis of tarsal tunnel syndrome is typically made by a podiatrist or a healthcare professional specializing in foot and ankle conditions. The diagnostic process involves a thorough evaluation, which includes the following steps:
- Medical History: The healthcare provider will begin by discussing the patient’s medical history. They will inquire about any symptoms experienced, their duration, and any relevant medical conditions or previous foot injuries.
- Physical Examination: A comprehensive physical examination of the foot and ankle is conducted. The podiatrist will assess for areas of tenderness, any visible signs of swelling or inflammation, and motor and sensory functions in the foot.
- Symptom Assessment: The patient will be asked to describe the nature and location of their symptoms, including pain, tingling, numbness, or weakness.
- Neurological Tests: Specific neurological tests may be performed to assess nerve function in the affected area. This can include testing reflexes, evaluating sensation, and assessing muscle strength.
- Tinel’s Sign Test: The Tinel’s sign test may be performed, where the healthcare provider gently taps over the tarsal tunnel area to see if it triggers symptoms like tingling or numbness.
- Provocative Maneuvers: The podiatrist may perform certain movements or maneuvers to provoke or exacerbate symptoms and assess the patient’s response.
- Imaging and Diagnostic Tests: In some cases, additional diagnostic tests may be ordered to confirm the diagnosis and assess the severity of nerve compression. These tests can include:
- Nerve Conduction Studies: Nerve conduction studies measure the speed and strength of electrical impulses in the nerves. Abnormalities can indicate nerve compression.
- Electromyography (EMG): Electromyography involves the use of needles to assess muscle activity in response to nerve signals, helping to identify nerve issues.
- Ultrasound: Ultrasound imaging can provide real-time images of the tarsal tunnel and surrounding structures, helping to identify any abnormalities or masses.
- Magnetic Resonance Imaging (MRI): MRI scans can offer detailed images of the tarsal tunnel and any structures that may be compressing the nerve.
How is tarsal tunnel syndrome treated?
When dealing with tarsal tunnel syndrome, healthcare professionals often initiate treatment with
conservative measures to relieve symptoms and reduce nerve compression. These treatment options can include:
- Rest and Activity Modification: Resting the affected foot and modifying activities that exacerbate symptoms, such as avoiding prolonged standing or walking, can provide relief.
- Footwear Modification: Wearing shoes with proper arch support and cushioning can help alleviate pressure on the tibial nerve. In some cases, custom-made orthotic devices may be prescribed to correct any biomechanical abnormalities in foot structure.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter or prescription NSAIDs may be recommended to reduce inflammation and alleviate pain. These can help manage discomfort associated with tarsal tunnel syndrome.
- Physical Therapy: Physical therapy exercises focused on strengthening the muscles in the foot and ankle, as well as improving flexibility, can play a crucial role in conservative management. A physical therapist can design a tailored exercise program to address specific needs.
- Supportive Bracing: In some instances, the use of ankle or foot braces may be recommended to provide additional support to the affected area and reduce strain on the tibial nerve.
- Immobilization: For more severe cases or when conservative measures have been ineffective, immobilization with a cast or walking boot may be employed to restrict movement and reduce nerve compression.
- Lifestyle Modifications: Adjusting one’s daily activities to minimize pressure on the foot, such as taking breaks and incorporating stretching exercises during prolonged periods of standing or walking, can be beneficial.
The specific treatment plan will be tailored to each individual’s needs and may involve a combination of these conservative approaches to achieve optimal results. The goal of conservative treatment is to alleviate symptoms, improve function, and reduce nerve compression without the need for surgical intervention.
Patients should work closely with their healthcare provider to determine the most suitable treatment plan based on their condition and response to conservative measures.
When is surgical intervention recommended for tarsal tunnel syndrome?
Surgical intervention for tarsal tunnel syndrome is typically considered in specific circumstances when conservative treatments have been ineffective or when the condition is severe and significantly impairs the patient’s quality of life. The decision to pursue surgical intervention is made on a case-by-case basis and takes into account various factors, including:
- Severity of Symptoms: When tarsal tunnel syndrome causes severe and persistent symptoms that significantly affect a patient’s daily life, surgical intervention may be recommended.
- Lack of Improvement with Conservative Treatment: If conservative treatments, such as rest, physical therapy, or orthotic devices, have not provided relief or have not yielded the desired improvement, surgery may be considered.
- Functional Impairment: When the tarsal tunnel syndrome results in functional impairment, including difficulty walking, standing, or performing regular activities, surgery may be necessary to restore function.
- Evidence of Nerve Compression: Diagnostic tests, such as nerve conduction studies, electromyography, or imaging studies, may reveal clear evidence of nerve compression within the tarsal tunnel, reinforcing the need for surgical intervention.
- Patient Preference: In some cases, patients may opt for surgery when they are not satisfied with the results of conservative treatment or wish to address the condition more definitively.
Surgical options for tarsal tunnel syndrome may include:
- Tarsal Tunnel Release: This procedure involves the release of the ligament forming the roof of the tarsal tunnel to alleviate compression on the tibial nerve.
- Mass or Cyst Removal: If a mass or cyst within the tarsal tunnel is causing compression, the surgeon may remove it to relieve pressure on the nerve.
- Nerve Decompression: In some cases, additional adjustments to the surrounding structures may be made to ensure optimal nerve decompression.
The specific surgical approach recommended will depend on the underlying cause, the severity of the condition, and the patient’s individual circumstances. It is essential for individuals considering surgery to consult with a skilled podiatrist or surgeon specializing in tarsal tunnel syndrome. This consultation allows for a comprehensive discussion of potential benefits, risks, and expected outcomes of surgical intervention, helping patients make informed decisions regarding their treatment.
What is the recovery process like after surgery for tarsal tunnel syndrome?
The recovery process following surgical treatment for tarsal tunnel syndrome can vary depending on several factors, including the extent of the procedure, the individual’s overall health, and their response to surgery. Here is an overview of the typical recovery process:
- Immobilisation: After surgery, the patient’s foot is often immobilized to allow for proper healing. This may involve the use of a cast, walking boot, or other supportive devices. The type and duration of immobilization will depend on the specific surgical procedure performed
- Weight-Bearing Restrictions: In the immediate postoperative period, weight-bearing on the affected foot is usually restricted. Patients may need to use crutches or a walking aid to keep weight off the surgical site. The duration of these restrictions can vary and is determined by the surgeon.
- Wound Care: Proper wound care is crucial to prevent infection and promote healing. Patients will receive instructions on how to clean and care for the surgical site. It’s essential to keep the wound clean and dry.
- Pain Management: Pain and discomfort following surgery are common. Patients are typically prescribed pain medications to manage post-operative pain. It’s important to take these medications as directed by the surgeon.
- Physical Therapy: Physical therapy and rehabilitation exercises may be recommended to improve strength, flexibility, and mobility in the foot and ankle. These exercises are crucial for a successful recovery.
- Gradual Resumption of Activities: Patients will receive guidance on gradually resuming activities. This may include a step-by-step plan to return to weight-bearing and normal daily activities. It’s essential to follow these instructions to avoid complications.
- Follow-Up Appointments: Regular follow-up appointments with the surgeon are necessary to monitor the progress of healing and assess the outcomes of the surgery. The surgeon may make adjustments to the treatment plan as needed based on the patient’s recovery.
The recovery period can range from several weeks to several months, depending on the complexity of the surgery and the individual’s response to treatment. It’s important for patients to adhere to the post-operative guidelines provided by the surgeon and attend all scheduled follow-up appointments. Any concerns, unusual symptoms, or complications should be promptly reported to the healthcare provider.
Throughout the recovery process, the goal is to regain mobility, alleviate pain, and improve function in the foot and ankle. Patients should be patient and diligent in following the recommended treatment plan to achieve the best possible outcome.
Are there any potential complications or long-term effects associated with tarsal tunnel syndrome?
While tarsal tunnel syndrome can often be effectively managed with conservative treatments or surgery, there are potential complications and long-term effects to be aware of:
- Recurrence: Tarsal tunnel syndrome may recur, even after successful treatment. This can happen if the underlying causes, such as flat feet or overpronation, are not adequately addressed. Patients should continue to follow preventive measures and lifestyle modifications to reduce the risk of recurrence.
- Surgical Risks: Surgical treatment carries inherent risks, such as infection, bleeding, or nerve damage. Although these complications are relatively rare, patients should be aware of them and closely follow post-operative care instructions to minimize these risks.
- Scarring: Surgical procedures may result in scarring at the incision site. While this scarring is usually minimal and well-tolerated, it can occasionally cause discomfort or cosmetic concerns.
- Nerve Damage: In severe cases, tarsal tunnel syndrome can lead to permanent nerve damage if left untreated for an extended period. Early diagnosis and prompt treatment are essential to prevent long-term nerve damage.
- Functional Impairment: In some cases, tarsal tunnel syndrome can lead to long-term functional impairment of the foot and ankle, particularly if the condition is not addressed in a timely and appropriate manner
- Chronic Pain: Persistent or recurring symptoms, despite treatment, can result in chronic pain in the foot and ankle, affecting an individual’s quality of life.
It’s important to note that with proper diagnosis, treatment, and adherence to post-operative care and rehabilitation, the majority of patients experience relief from tarsal tunnel syndrome and a return to normal foot function. To minimize the risk of complications and long-term effects, individuals should seek prompt medical attention and follow their healthcare provider’s recommendations for treatment and lifestyle modifications.
Regular follow-up appointments and ongoing foot care can help monitor and manage any potential complications or long-term effects associated with tarsal tunnel syndrome.
Can tarsal tunnel syndrome be prevented?
While it may not always be possible to prevent tarsal tunnel syndrome entirely, especially if there are inherent structural or anatomical factors, there are several preventive measures that individuals can consider to reduce the risk of developing this condition or to prevent its recurrence:
- Proper Footwear: Wearing shoes with good arch support and cushioning can help distribute pressure evenly across the foot and reduce the risk of nerve compression. Avoid shoes that lack support or have worn-out insoles.
- Orthotic Devices: For individuals with flat feet or overpronation, custom-made or over-the-counter orthotic devices can provide additional arch support and help correct biomechanical abnormalities.
- Activity Modification: Be mindful of activities that put repetitive stress on the foot and ankle, such as running or standing for extended periods. Take breaks, incorporate stretching exercises, and avoid overexertion.
- Maintaining a Healthy Weight: Excess body weight can increase pressure on the foot and exacerbate tarsal tunnel syndrome. Maintaining a healthy weight through diet and exercise can reduce this risk.
- Lifestyle Modifications: If you have an underlying condition such as diabetes or arthritis, proper management and lifestyle modifications are essential to maintain overall foot health and reduce the risk of nerve compression.
- Regular Foot Examinations: Pay attention to any signs or symptoms of tarsal tunnel syndrome, such as pain, numbness, or tingling in the foot. Early diagnosis and treatment can prevent the condition from worsening.
- Proper Warm-Up and Stretching: Before engaging in physical activities or exercises, ensure you warm up and stretch the foot and ankle muscles. This can help prevent overuse injuries that may contribute to tarsal tunnel syndrome.
- Foot Posture Awareness: Be aware of your foot posture and gait. If you notice any abnormalities or discomfort, consult with a podiatrist for evaluation and recommendations.
- Regular Foot Care: Maintain proper foot hygiene and care to reduce the risk of infections or other foot conditions that could indirectly contribute to tarsal tunnel syndrome.
It’s important to remember that preventive measures can vary depending on an individual’s specific risk factors and circumstances. If you have concerns about tarsal tunnel syndrome or if you believe you are at risk due to your foot structure or activities, consult with a healthcare provider or a podiatrist. They can provide personalized guidance and recommendations to help reduce the risk of tarsal tunnel syndrome and promote overall foot health.
Take care of your feet with Hurst Podiatry
Tarsal tunnel syndrome can be a debilitating condition that affects the foot and can significantly impact daily activities. At Hurst Podiatry, our dedicated team of experienced podiatrists understands the challenges associated with tarsal tunnel syndrome and is committed to providing personalised and comprehensive care.
If you are experiencing symptoms of tarsal tunnel syndrome or have concerns about your foot health, please schedule a consultation with us and take the first step towards finding relief and regaining your mobility.