Understanding Iliotibial Band Syndrome
Even though the feet may be far away from other areas of the body, certain factors to do with your feet and the way you take care of them can impact the rest of the body.
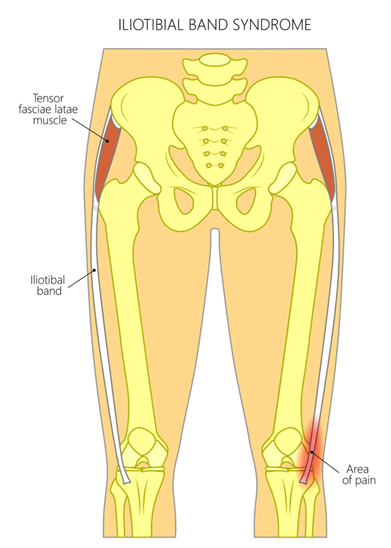
One condition that the biomechanical make up of your feet could have an impact on is known as Iliotibial band syndrome. This condition manifests in irritation and inflammation of the thigh, usually all the way from hip to shin.
In this article, we’re going to focus on this condition and also discuss how your feet can impact it.
What is Iliotibial Band Syndrome?
Iliotibial band syndrome (ITBS) refers to inflammation and irritation of the thick band of tissue that runs down the outside of the thigh from the hip to the shin. This tissue band is known as the iliotibial band or IT band. It plays an important role in stabilising the knee during physical activity.
However, repetitive movements like running can cause the IT band to become irritated. This results in pain and inflammation around the outside of the knee – the primary symptom associated with ITBS.
What Causes ITBS?
ITBS usually flares up due to repetitive stress on the iliotibial band from certain knee and hip motions during exercise. Running, cycling, hiking, climbing stairs, dance, aerobics, and other sports are common triggers. Any exercise that causes repeated knee flexion can strain the IT band at the knee attachment point.
Contributing factors include:
Biomechanical Factors:
These factors disrupt proper leg and foot alignment, placing uneven stress on the IT band with activity.
Muscle Imbalances & Weaknesses:
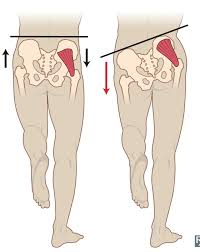
- Poor hip abductor and glute strength – If these muscles are weak or imbalanced, other structures like the iliotibial band have to work harder to stabilise the hip and knee during motions like running. This strains the tissue.
Improper Training:
- Sudden increases in activity, distance, speed, or duration – Too much-too soon can overload the connective tissues faster than the body can strengthen them.
- Excessive downhill running / Descending on hikes or trail runs Downhill grades increase load and injury risk for the quads, hips, and knees.
- Running on uneven or slanted surfaces like cambered roads – this creates imbalance and additional frontal plane forces through the lower limb joints and soft tissues.
Poor Technique / Movement Faults:
- Overstriding when running
- Limited hip internal rotation when leg swings back – restricted movement can load the iliotibial band greatly during stride propulsion.
Equipment & Environmental Factors:
- Worn or incorrect footwear
- Hard running surfaces
ITBS Signs & Symptoms
The main sign is pain over the outside (lateral aspect) of the knee. This pain usually worsens with activity.
Common symptoms include:
- Lateral knee pain when walking, running, squatting, going upstairs, sitting for long periods
- Outside knee pain that flares up after exercise rather than during
- Pain or tenderness directly over the iliotibial band as it crosses the knee
- Pain running from the hip down the outside of the thigh to the knee and shin
Later signs as the condition progresses:
- Visible tightness/tension in the iliotibial band
- Swelling on the outside of the knee
- Crepitus – Grating sound from inflammation under the IT band
- General knee stiffness, difficulty straightening the knee
- Weakness or compensation patterns in surrounding muscles
It’s crucial to address signs early before compensations lead to secondary issues elsewhere. Listen to warning signs from your body.
Risk Factors for ITBS
Certain anatomical, biomechanical, muscle imbalance, and training factors raise injury risk, including:
- High foot arches (underpronation)
- Leg length discrepancy
- Overpronation / feet excessively rolling in
- Weak hip abductors, gluteal and core area
- Tight iliotibial band, quads, hip flexors
- Poor running technique and biomechanics
- Hill running or descending exercises
- Sudden spikes in activity or mileage
- Hard or uneven running / walking surfaces
- Worn out athletic shoes
- Bowlegged alignment (increased Q-angle)
- Femoral anteversion – inward angling femur bone
- External tibial torsion – outward turned tibia
Addressing these factors through proper strength & flexibility training, nutrition for muscle repair, technique cues, equipment, surfaces, and load management is key for prevention.
IT Band Syndrome Conservative Treatment
Most cases of IT band irritation respond very well to conservative treatment methods:
Rest & Ice
This reduces inflammatory response critical in early stages. Apply ice bags wrapped in thin towel for 10-15 minutes after activity when symptoms flare up.
Anti-inflammatories
NSAID medication and creams calm pain signals and control inflammation short-term while tissue heals. Always follow directions.
Specific stretches and strengthen moves rebalance muscle groups and joint alignments. This alleviates pressure on the IT band long term. Target key areas like the IT band, lateral thigh muscles, hips, glutes, quads, calves. Use dynamic movements that integrate the whole kinetic chain. Focus on flexibility, mobility, coordination, stability and movement quality.
Massage, Foam Rolling, Fascial Tools
Using manual pressure and myofascial release aids restore supple soft tissue and relaxed muscles. Boosts blood flow to speed healing too.
Proper Footwear / Orthotics
Supportive athletic shoes designed for your foot type help alignment and impact absorption. Custom orthotics aid biomechanical issues. Replace shoes regularly.
Identifying faulty motions during gait, squatting, hinging patterns helps implement fixes to offload the IT band.
Kinesiology Taping
Strategic hypoallergenic tape lifts the skin gently which assists proper realignment of overworked structures like the IT band and surrounding muscles and fascia after injury. Fosters proper movement patterning. Augments other therapy.
Corticosteroid Injections
For moderate ITBS cases unresponsive to conservative care methods for over 3 months, an injection of anti-inflammatory steroid medication combined with local anaesthetic can reduce inflammation considerably associated with chronic IT band friction. Most effective injected directly around the painful area near the lateral knee soft tissues. 3 injections spaced 1 month apart is common protocol.
Injury Prevention Strategies
Several proactive tips minimise ITBS injury recurrence including:
- Gradually progress any activity increases – you can learn more about why you might want to visit a podiatrist before starting a new exercise regime here.
- Include consistent hip and gluteal strengthening
- Perform regular foam rolling / stretching hip to shin
- Maintain optimal nutrition and manage weight
- Wear appropriate athletic shoes for individual foot mechanics and replace regularly
- Get gait evaluations to correct imbalanced movement patterns
- Incorporate cross training routines with less impact loading
- Improve running and movement technique – shorten stride, avoid overstriding, increase cadence
- Pay attention to body’s warning signs during rehab and adjust accordingly
With a slow graded return to activity program guided by skilled providers and attention to prevention strategies, full rehabilitation form IT band syndrome is highly likely.
When to Seek Further Treatment
If symptoms have not resolved substantially in 6 weeks with conservative measures, consult an orthopaedic doctor or sports physician for imaging tests to rule out other knee joint or cartilage issues. They can assess if advanced modalities like shockwave or platelet rich plasma injections, surgery or other methods beyond home care may be warranted depending on the severity of damage sustained.
The small percentage of patients with lasting symptoms unresponsive to 6 months of properly progressing therapy may require surgical invention like IT band removal, bursectomy or lengthening procedures.
Surgical Options for Chronic Treatment-Resistant ITBS
For the ~ 1% of patients where thorough conservative therapy fails and disability persists for more than 6 months, certain surgical approaches can provide relief when all other options are exhausted.
Common approaches include:
Iliotibial Band Bursectomy
Involves surgically removing inflamed problematic bursa tissue to minimize friction on the lateral knee with motion. This area can become severely irritated with repetitive IT band motion across the bone near the joint line.
Iliotibial Band Tenotomy
The IT band tightness and stiffness is surgically incised near where it crosses the knee joint for greater flexibility. This is performed in cases with very restricted IT band excursion limiting normal function despite prolonged rehab efforts.
Iliotibial Band Release
In some instances, a section of the IT band may be completely excised and removed. This alleviates pull along the thigh and strain on the knee attachment point. It is reconstructed and sewn based on tension mapping to restore function. This allows for greater mobility long term without sacrifice to stability.
All surgical options should only be performed after thorough conservative therapy has been undergone for over 6 months without desired pain relief or mobility gains. Surgery aims to remove isolated damaged tissue while preserving healthy structures that maintain proper biomechanical forces through the hip to foot kinetic chain.
Post operative therapy focuses on safely restoring flexibility, strength, neuromuscular control, and cardiovascular reconditioning based on surgeon guidelines and directives for tissue healing stages. With dedication and patience to the rehab timeline, individuals can return to full activities in most cases following surgery.
Conclusion
Iliotibial band syndrome is a common source of lateral knee pain in active populations, especially runners. Understanding the various causes, risk factors, symptoms, and treatment options is key to effectively managing this condition.
Most cases of IT band irritation resolve well with conservative treatment methods like rest, anti-inflammatories, physical therapy, taping, footwear modifications, injections, and gradual return to activity. Prevention is ideal through strength and flexibility training, proper mechanics, equipment, and smart training practices.
Though frustrating to deal with, this overuse injury responds very favourably to a targeted rehabilitation program when addressed proactively at early stages. Only about 1% of individuals end up needing any form of surgery if conservative care is robustly implemented for an adequate trial period.
Being aware of risk factors, listening to warning signs during exercise, and adjusting activity levels appropriately can help active individuals continue participation in meaningful activities through the lifespan. With some care and minor adaptations, full recovery from iliotibial band syndrome is highly achievable.
Take care of your feet with Hurst Podiatry
As we mentioned earlier, your feet can impact a lot of areas of your body, and if you’ve noticed any pain or discomfort, like we’ve described today, you should come see us at our Podiatry clinic.
We can assess your foot health and put you on the right road to recovery. We have three clinics you can visit, including two in Healesville and one in Kilsyth. Book your consultation here.